Mississippi State CFD Expert is Designing New Artificial Lung Device
April 3, 2017
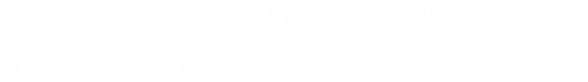
A computational rendering of an artificial lung
created with computational fluid dynamic software.
Designed by CAVS Biomedical Researcher and Designer
Greg Burgreen
created with computational fluid dynamic software.
Designed by CAVS Biomedical Researcher and Designer
Greg Burgreen
Children with acute and chronic lung diseases must often wait months or even years for a lung transplant. While in the hospital, the existing equipment used to help them breathe is large, immobile, and can worsen their condition by overtaxing already damaged lungs. Children are also confined to their beds and prevented from moving around which can contribute to worsening their physical and mental states.
The device that Burgreen is prototyping with Mississippi State University computing resources is called the Pediatric Paracorporeal Assist Lung or P-PAL and is a small (about the size of an average adult fist), efficient device that would stay exterior to the body while tubes connect to blood vessels to assist circulation and pulmonary functions. During this process, the device oxygenates the blood, removes carbon dioxide, and returns it to the patient.
Though invasive (the tubes are inserted either through the femoral artery or the jugular vein), the device would allow patients to be mobile during their treatment and survive indefinitely while waiting for a lung transplant.
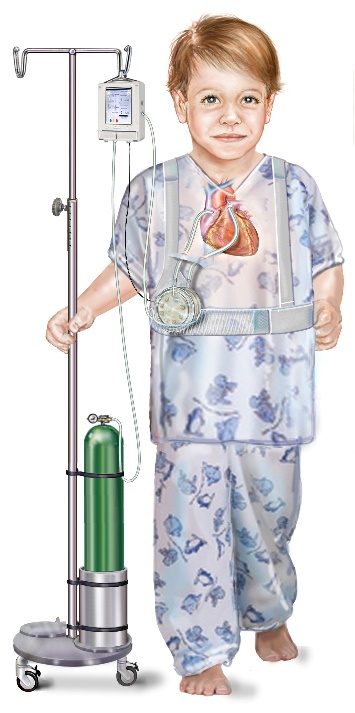
A medical sketch of a young patient
using a portable artificial lung.
Photo provided by Greg Burgreen
using a portable artificial lung.
Photo provided by Greg Burgreen
However, the past 20 years has seen the adoption of computational prototyping which is significantly faster, cheaper, and aids in improving researchers' understanding of device operation.
Burgreen surmises that without Mississippi State's input, "The project has the potential to languish in the early design phase grappling with poorly performing devices that would unnecessarily divert project resources away from the later planned animal trials. By developing devices faster, cheaper and optimized by computational guidance, Mississippi State University is helping to improve and prolong the lives of children suffering from lung diseases."
Though clinical use for patients is years away, Burgreen believes the P-PAL could be a major therapeutic improvement if not a full treatment for children with lung diseases. However, there are drawbacks.
Research obstacles include finding efficient ways to oxygenate the blood without the device causing damage to red blood cells. Burgreen states one of the hardest things in this type of research is trying to mimic the sophistication and efficiency of human physiology without causing mechanical damage to blood.
If the research team can overcome these obstacles and design the P-PAL to work for adolescent patients, then the miniature technology can be translated to benefit adults suffering from lung disease. Having secured NIH funding for the next few years, the MSU and UoP multi-disciplinary team continues to leverage MSU's computational expertise and state of the art computing facilities to help improve and prolong the lives of children suffering from lung diseases.
Written by Shun Pounds, Technical Writer for HPC2 Publishing Group.